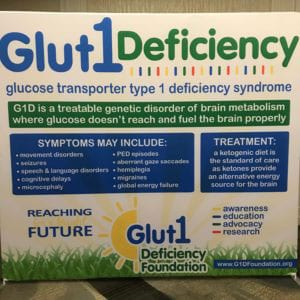
I had the pleasure of attending the Glut1 Deficiency Foundation’s 2019 Conference. While this article can’t possibly do the event justice and encompass all it had to offer, we will attempt to showcase some of the highlights.
The conference began with a presentation by Dr. De Vivo, an expert in his field. Dr. De Vivo stated that he continues to learn about Glut1 and its true impact and implications from the families he cares for. He provided a general overview in the history of Glut1 and clarified that, while the standard of care is the prescription of the ketogenic diet, it is a symptomatic therapy. There is no currently approved disease modifying treatment available. He stated that Glut1 involves “a complex phenotype that requires a multidisciplinary approach.”
Dr. Jorg Klepper stated that outcomes in Glut1 are not solely based on the type of genetic mutation but also the age at which an individual is diagnosed and begins treatment. He encouraged the audience to join the Glut1 registry in order to help advance research, saying; “we need you, as the experts, to tell us about what’s going on with your children, and then we can do the research.”
Dr. Michel Willemsen is conducting research to better understand why 10-20% of people with Glut1 do not respond well to the ketogenic diet and to see if an infusion of lactate could be beneficial.
Dr. Toni Pearson provided an overview of movement disorders in Glut1 Deficiency. Movement disorders are common in those with Glut1 but can vary from person to person and can include both persistent and episodic presentations. Persistent disorders may include spasticity, dystonia, and ataxia, while the episodic movement disorders that may occur include weakness, involuntary movements, and episodic eye-head movements in infancy. The movement disorders in Glut1 can lead to individuals being misdiagnosed with cerebral palsy.
Dr. Veronica Hinton’s presentation “Cognitive Considerations in Glut1 Deficiency” highlighted that those with Glut1 may have stronger receptive language skills than expressive language skills, and could benefit from speech therapy. The difficulty with expression can be a source of frustration for children, who most likely understand more than they are able to convey to others. Those with Glut1 may need help learning to focus on details and could be helped by a step by step review of schoolwork and partaking in things like visual search puzzle games and word searches. Physical and occupational therapy can assist people with Glut1 work on their fine motor skills. Dr. Hinton suggested using teaching strategies that are step by step and to utilize repetition. She stressed that both children and adults with Glut1 can continue to learn, and, if on the correct diet, will most likely not lose learned skills over time. She echoed the sentiment that the earlier the diet is started, the better, and stated that attention spans, verbal skills, and test scores tend to improve after the implementation of the diet. She encouraged families to help their children become more independent, as learning adaptive behavior for daily living skills can help them increase their overall confidence and assist them in achieving even more.
 Dr. Kossoff discussed how 2018 saw a huge increase in interest in the Ketogenic diet resulting in a record number of publications. He presented highlights of the revised international consensus paper for the treatment of Glut1, including the almost unanimous agreement that the ketogenic diet should be started as early as possible, even before the observation of seizure activity. Dr. Cervenka continued the presentation regarding the ketogenic diet and its new popularity with some words of caution. The growing interest in the diet by the general population has made more food options available to those with Glut1, but Dr. Cervenka warns that many products may be marketed as ketogenic as a selling point, but may not actually adhere to the diet.
Dr. Kossoff discussed how 2018 saw a huge increase in interest in the Ketogenic diet resulting in a record number of publications. He presented highlights of the revised international consensus paper for the treatment of Glut1, including the almost unanimous agreement that the ketogenic diet should be started as early as possible, even before the observation of seizure activity. Dr. Cervenka continued the presentation regarding the ketogenic diet and its new popularity with some words of caution. The growing interest in the diet by the general population has made more food options available to those with Glut1, but Dr. Cervenka warns that many products may be marketed as ketogenic as a selling point, but may not actually adhere to the diet.
Dr. Cervenka also presented the results of a survey taken by adults with Glut1 or their caregivers. She found that there is a variety of symptoms, abilities, and responses to treatment. That said, those on the ketogenic diet were more likely to be free of seizures. She found that emotional stress can trigger symptoms and that physical activity may reduce them. She concluded that there is room for improvement regarding the care of adults with Glut1, including an increase in education for adult neurologists, increasing the availability of various types of therapies, and the facilitation of employment for patients. Dr. Cervenka is continuing to study Glut1 in adults considering things like the impact of hormonal changes on Glut1 symptoms, and what long term monitoring should be in place.
Wesley Lowman, RDN, LDN, gave a presentation on how to successfully stick to a ketogenic diet. His first “key component” is a well-defined care team comprised of a dietitian, their physician, fellow caregivers, and a social support network. The second component is a comprehensive pre-diet clinic in which the current diet is reviewed, along with medications, and dietary goals are discussed, as well as their social implications. Lowman argued that the 3rd key component for success is routine follow up appointments in order to monitor lab work and symptoms. These factors are meant to ensure that the ketogenic diet as a therapy is both effective and practical and progress is tracked.
Several mothers of “keto kids” led a breakout session that provided some specific guidance for a ketogenic lifestyle at home. Dawn Martenz’s daughter is on the ketogenic diet and she worked extensively with the Charlie Foundation and developed ketogenic cookbooks. Her daughter has been on the ketogenic diet for about 10 years now, and the family has a system down pat. She suggests keeping meals simple, admitting “There is nothing that feels simple about keto at first. It feels overwhelming and confusing.” She advises others to keep easy recipes on index cards and staple ingredients in the house at all times. Many of her go-to recipes do not require cooking, and that, in addition to color coded containers to outline amounts of protein, fat, fruit etc, allow her children to be independent in creating their own meals while adhering to the diet.
Dawn is also a big advocate of meal prepping. She will create large quantities of keto meals and freeze them pre portioned for the week ahead. She also feels that involving family and friends can make a big difference. She has found that people would like to help and asking them can yield great results and adapted recipes. Dawn’s family has even had positive outcomes asking for adjusted meals at restaurants. She feels it’s also a good idea to research what would be straight forward options at several different establishments and to have some prepackaged, pre-researched, foods that are easy buys for trips.
Dawn’s concluding message was to continually consult with a dietitian as the diet will need adjustments over the years, to help children move towards independence, and to address compliance issues. She states that the ketogenic diet is more of a lifestyle for those with Glut1 than it is a diet, because it doesn’t have an end in sight.
Maria Rebbecchi’s son has been on the diet for 6 years and she has found some creative ways of providing him with ketogenic sweet treats, after having difficulty finding options in stores. She suggests making snow cones with shaved ice and sugar free flavoring or diet sodas, or using the same concept in ice pop molds. She recently discovered that buying a rolled ice cream kit, yields easy keto ice cream with heavy cream and sugar free Hershey’s syrup. Maria also makes keto gummy candies with gelatin and sugar free Jello flavoring. In the past, adding supplements to these gummies have made it easier for her son to get the vitamins he needs. She’s found that edible glitter can be substituted in place of sprinkles for 0 carb decorations. Her son also enjoys taco shells made entirely from cheese, and fried veggies coated with egg and cheese instead of breading. Popcorn flavoring can be used to season macadamia nuts for a new version of a go-to snack. Some of Marie’s go-to products are a magic bullet to create keto smoothies for easy breakfasts, and an immersion blender for mixing cream and oil. She recommends investing in dependable containers to prevent leaks in transport and easy travel items such as crystal light packets, or Quest protein chips.
Kelly Jones shared her family’s experience with a feeding tube. Her son really struggled with the ketogenic diet. Compliance to the diet involved a fight every day. He found it difficult to drink the amount of cream he needed, gagging or vomiting if he drank it quickly. It was something he dreaded. One day Kelly brought home a book about G-tubes, meant to explain the process of tube feeding to children, and a book of photographs displaying children with G-tubes, engaged in fun activities. She told her son that if he were to get a G-tube, he would no longer have to drink his cream. She had found a lot of support and the book recommendations from other families over social media. She thought it might be a good option for her child.
Her son expressed enough interest, without her pushing, that she scheduled a call with a surgeon. Kelly let him (age 10) speak directly to the physician. He asked if he could still go swimming with the tube, and was happy to hear that he could.
Kelly continued to speak to other families and was sent a video of another child using their tube. When her son saw it, he said, “That’s it?” He was amazed at how quick and simple feedings could be. He decided he wanted the surgery. Kelly did her best to make it a positive experience for him. She created a chart to countdown to the surgery with pictures of cartons of whipping cream on each day that he could rip off as the date approached.
The G-tube has taken some getting used to; they had to make adjustments for how many meals he would have based on how much oil he could tolerate at a time. It has overall been an improvement. Her son has gone on to make a video of him using his tube for other families to see and learn from. Kelly recommended a toiletry bag for traveling with supplies and a Boon patch drying rack for syringes.
Leslie Holleman’s son was put on a modified ketogenic diet therapy which helped him to become more independent. Her family uses color coded measuring cups and recipe cards laid out to encourage him to put together his own meals while staying compliant. The Charlie Foundation was a good resource for them to convert grams to measuring cups, and Leslie’s son is able to track his meals in a notebook daily. Leslie urged the audience to empower their loved ones by actively involving them in decision making and to celebrate small successes and progress. She suggested a positive approach to learning and this sentiment was echoed in a general session’s presentation by Dana Pottschmidt.
Dana Pottschmidt, MSW, LSW, RBC, stated that in order to foster more independence, families should focus on the strengths and abilities of their children, rather than the areas they may have difficulty. She suggests creating short term personal goals and continually encouraging your child towards them. Some examples of overall goals to be achieved through fostering independence included things like independent living skills, emotional and physical self-care, diet management, and employment. Dana’s presentation revolved around the development of structure and routine so that those living with Glut1 know what to expect and can refer to things like a visual schedule and checklist. She advocates for patients to be involved in meal planning with coinciding explanations of what is being done and why. She also is a proponent of self-reporting –suggesting a phone battery analogy so children and adults can communicate what their energy levels are. Technology can assist with these involvements through task lists apps or diet tracking apps.
In addition to providing scientific updates and daily living tips, the event offered comradery and solidarity for families who had traveled from all over the world. Despite the variety of symptoms and impact of Glut1, overarching similarities and the difficulty of navigating a therapeutic ketogenic diet, fostered fast bonds and readily offered support between families. The event featured those living with Glut1 front and center, with a “red carpet” event to highlight individual’s and their stories, and family centered activities. The Glut1 Deficiency Foundation’s next conference will be held in 2021 in San Diego, click here to learn more about the event, and the organization behind it.
Share your stories, thoughts, and hopes with the Patient Worthy community!



