Visual hallucinations have been a known symptom of Parkinson’s disease for a long time, but the cause has evaded medical professionals. That is, until now. A recent study, titled “Visual Hallucinations in Parkinson’s Disease are Associated with Thinning of the Inner Retina,” has connected this symptom to retinal issues.
About Parkinson’s Disease
Parkinson’s disease is a progressive disorder that affects the central nervous system (CNS). It is characterized by its effect on movement through five different stages. As the disease progresses, severity increases.
- Stage one is characterized by subtle tremors on one side of the body.
- In stage two symptoms are more noticeable, with tremors and rigidity on both sides of the body.
- Stage three brings loss of balance and slowed movement.
- Stage four makes it impossible for one to live independently.
- Stage five is the most severe, as patients cannot stand or walk. Hallucinations and delusions are common symptoms of this stage.
Parkinson’s disease occurs due to the death of motor neurons, some of which produce dopamine. Dopamine is important in the transmittance of messages to the muscles from the brain, so the loss of dopamine results in the loss of motor functions. Abnormal brain activity occurs when these neurons are lost. Doctors do not know why these motor neurons die, but they do suspect a few factors that play a role, such as genetics, environmental factors like toxins, and Lewy bodies.
Retinal Thinning in Parkinson’s
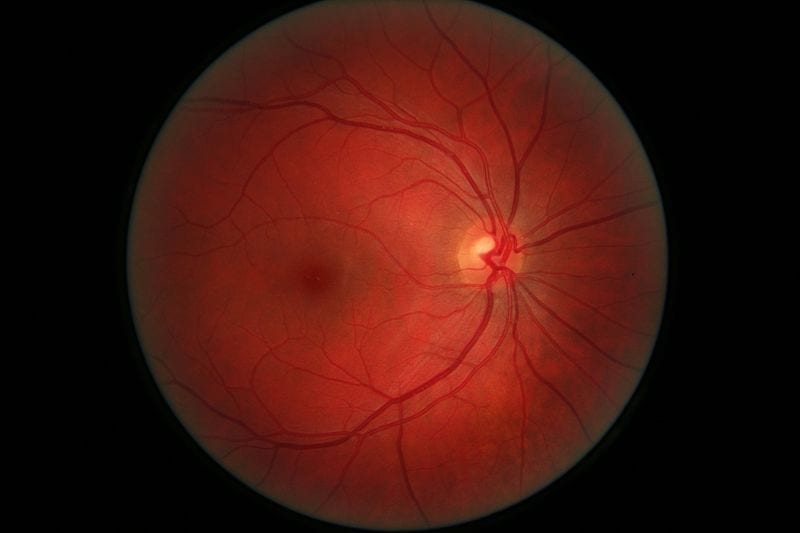
Medical professionals have been aware that Parkinson’s patients experience hallucinations and the thinning of the inner layers of the retina. In fact, past studies have demonstrated that there is a lack of dopamine paired with an accumulation of abnormal alpha-synuclein protein in the retina. They lead to thinning. However, this thinning had not been associated with the visual hallucinations that affected individuals experience.
About the Study
Researchers from the Onze Lieve Vrouwe Gasthuis (OLVG) Hospital in the Netherlands conducted a study to investigate the link between retinal thinning and hallucinations in Parkinson’s. They focused specifically on two inner layers of the retina: the inner plexiform layer and the ganglion cell layer. Their goal was to discover a link between visual acuity due to thinning and visual hallucinations.
In order to accomplish this goal, 40 Parkinson’s patients and 22 healthy controls were enrolled in a study. Every participant underwent an interview with a neurologist and an eye examination. After these, 14 patients were determined to experience hallucinations. Seven of these 14 hallucinated every single day, 25% every week, and the remaining 25% every month. The interview also revealed that these patients had more cognitive impairment and progressed symptoms.
After investigation, researchers discovered that there were no significant difference between the two layers of the retina in Parkinson’s patients and the healthy controls. However, the Parkinson’s group did have lower visual acuity.
Looking deeper into the Parkinson’s group, the thinning of the two layers was associated with visual hallucinations. This association remained even after researchers adjusted for age, cognitive function, disease stage, and LED; however, the association was non-significant. When age was taken into consideration, researchers could no longer find a relationship between worse vision and hallucinations.
In terms of global cognitive function scores (MoCA), retinal thinning was associated with lower scores. Later disease stage, more hallucinations, worse visual acuity, and increased thinning of the retina were all found to have a relationship as well.
In the end, more research is definitely needed into this topic. You can find the source article here.