Sickle Cell Anemia
What is sickle cell anemia?
Sickle cell anemia is the most well-known and severe of the sickle cell diseases (SCD).
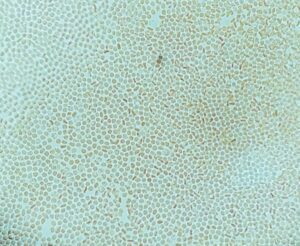
Normally, the protein hemoglobin, which is located on red blood cells, carries oxygen steadily through the body. However, with sickle cell anemia, sickle hemoglobin (hemoglobin S) causes strands to form that distort and stiffen red blood cells. Without their usual flexible shape, these crescent-like “sickle cells” get caught along vessel walls, creating blockages and halting the flow of oxygen.
In addition to causing blockages, sickle cells have shorter life cycles than regular red blood cells, reducing expectancy from around 120 days down to 20. Unable to produce new cells at a fast enough rate to match the deterioration of the old, people with sickle cell anemia have lower blood cell counts, hence the “anemia.”
Sickle cell anemia is chronic, but the severity of the condition differs depending on the person.
What causes sickle cell anemia?
Sickle cell anemia is an inherited disorder, wherein mutated genes give the body faulty instructions regarding the production of hemoglobin, causing sickle cells to form.
In the United States, about 100,000 people have an SCD. Sickle cell anemia is particularly common in the black community, with 1 in 13 African-Americans having at least one sickle cell gene, called sickle cell trait. A child with sickle cell trait becomes a carrier; while he/she would produce some sickle cells in the body, carriers often fail to have symptoms. They can, however, pass the condition on to their offspring. A child must receive two mutated genes (one from each parent) to develop sickle cell anemia, and there is a 25 percent possibility of this occurring. Thus, genetics is the cause of sickle cell anemia.
How is sickle cell anemia diagnosed?
Doctors can use a blood test to see if you are either a carrier or living with sickle cell anemia. They make a diagnostic determination based on the type of hemoglobin found, as hemoglobin S marks sickle cell anemia.
In newborns, doctors gather this blood sample by doing a “heel prick.” Sickle cell anemia testing is part of required newborn screening in the United States, but parents can have their children tested prenatally as early as 8-10 weeks into pregnancy. The latter would look at the hemoglobin gene rather than the hemoglobin itself.
What are the common symptoms of sickle cell anemia?
People are born with sickle cell anemia, but symptoms don’t appear immediately. Infants usually won’t develop problems until they’re around four months old, with the earliest signs being:
- Painful foot and hand swelling
- Fatigue or fussiness
- Yellow tones to the skin or eyes (jaundice and icteris)
As the child continues to grow, one major symptom is episodes of sharp, throbbing pain. These episodes can last hours or weeks, can be intense or moderate, and any part of the body may be affected. If severe enough, hospitalization may be necessary.
Beyond that, symptoms vary, but common ones include:
- Regular infections
- Delayed puberty
- Vision problems
- Mild to severe anemia
- High blood pressure in the lungs (pulmonary hypertension)
- Organ damage (lung, spleen, brain, liver, heart)
What treatment options are available for sickle cell anemia?
Hematopoietic stem cell transplantation (HSCT) is considered a cure for SCD, but it does have its challenges. Because of the difficulties finding an appropriate marrow donor, HSCT rates are low. Even when a donor is found—usually within the family—those who get a transplant often deal with complications like the risk of infection or stroke.
In the meantime, working closely with a hematologist to manage and prevent symptoms, as well as getting all recommended immunizations, will help people with sickle cell anemia live fully.
Where can I find more information about sickle cell anemia?
- American Society of Hematology
- National Heart, Lung, and Blood Institute
- Sickle Cell Disease Association of America
Sickle Cell Anemia
Sickle Cell Disease: Two Drugs are An Arm’s Length from a Potential Cure

Cured of Sickle Cell Disease, His Next Challenge was Mt. Kilimanjaro


Thalassemia and Sickle Cell Patients in the UK Gain Access to Blood Transfusion Test to Reduce Side Effects

Guideline-Based Care Might Reduce Cerebrovascular Illness in Sickle Cell Disease

U.K. Health Authorities Grant Approval for a New Medicine using CRISPR Gene Editing to Treat Beta thalassemia and Sickle Cell

Teaching the Human Body to Cure Sickle Cell Disease




