‘The future is here, it’s just not very evenly distributed’ William Gibson
These days there’s much more literature about mal de debarquement syndrome (MdDS) and this resource gives excellent information about the condition and the plans for future research – exciting times. However, a member of the UK group wrote that having MdDS is an exercise in resilience and all along I’ve been interested in the lived experience of MdDS as well as the science behind it. No one would wish MdDS on anyone but it has taught me a lot so I’m grateful to Patient Worthy for offering me the chance to reflect on what I’ve learnt.
1. Our researchers are awesome. When I joined the patient groups people were talking about job losses or loss of career progression; inability to study effectively; difficulties with looking after dependents; loss of healthy social lives; financial difficulties; struggles with people who think it’s all in our heads; and gaslighting from doctors. This causes psychological damage and similar issues that are common for people with invisible conditions and get reported by women in many areas of health. While we shared life-hacks and discussed what made our symptoms fluctuate, few of us dared to believe that there would be treatments available in our lifetimes. Yet, despite the immense challenges involved with researching rare conditions, we’re now at the point where the MdDS researchers hope to compare two treatment protocols to see which works best for the different subsets – and they aim to develop new treatments. Some of the team at Mt Sinai were part of a consortium of clinicians and researchers who won the Frontiers in Science Award, partly as a result of their work on MdDS. This program is their prize.. I’ve emailed the organizers to find out if the transcripts will be freely available to patients so that we can work with our healthcare systems to develop guidelines so that this part of the future can get distributed more evenly.
2. From working with patient advocates in the rare conditions space I’ve learnt that many patients get labelled with vague psychiatric conditions during their diagnostic odysseys. It’s rare that I attend rare conditions events and don’t meet someone, usually female but not always, who hasn’t been traumatized by being told that if they don’t accept the psych labels (‘functional’ aka ‘medically unexplained symptoms’ being a common one) their primary care support will be removed. No-one can agree what ‘functional’ means and I am aware that the ambiguity seems deliberate (for more about this issue, click here.) This doesn’t shout good practice or Health 3.0 to me, but this does:
“A diagnosis of somatic symptom disorder implies that the pain is caused by a behavioral, that is, mental condition. However, it is not appropriate to diagnose individuals with a mental disorder solely because an alternative medical cause cannot be established,” Jaochim Scholtz, MD, an IASP task force member, explained in Practical Pain Management.
This is from the WHO announcement about pain being recoded, but it’s equally applicable to all physical symptoms and is part of a better future too.
Other doctors are speaking up about these issues and I’m interested to note that it is often doctors who work with patients with rare conditions who do so. Prof Grahame, discussing Ehlers-Danlos syndrome, points out the high-risk strategy involved with the belief that ‘medically unexplained symptoms’ are psychogenic in origin. Dr Emma Reinhold discusses the need to move from ‘MUS’ to ‘DEN’ (doctors educational needs) so that patients unmet needs get met.
3. Provision for people with rare conditions, in terms of patient engagement and empowerment, is brilliant in the UK and has a bright future. I did a risk/benefit analysis with my GP before travelling to attend any rare conditions events/training and we decided that the benefits would outweigh the risks and this has proved true. This type of provision is available in other countries – to a greater or lesser extent – but I feel for people with MdDS in larger countries where the travel times are longer and so could be more risky. Thankfully much of the information we need is available via toolkits and patient portals and, for those who find scrolling difficult, adaptive technology such as screen readers are our friends. But the exchange of ideas and solution-focused brainstorming at the events is invigorating and getting to the venues gives my spatial awareness system a good work-out, which it needs.
4. My GP and neurologist are excellent and I consider myself lucky to have them in my corner. Since I can’t clone them for everyone with rare conditions, I talk up their good practice whenever I get the chance since once we know what good looks like, it’s easier to find and have better futures. My trust in the medical profession was broken in the early years of having MdDS and even though they can’t treat, cure or reassure me, they’ve given me that trust back – and that rocks.
Polly Moyer
Co-founder of Action for Mal de Debarquement Syndrome UK
Action for MdDS UK
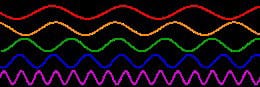
Technology Training Treatment