Editor’s Note: Chronic conditions and rare diseases don’t discriminate. Patient Worthy and its partners are interested in amplifying the voices of those from all identities and backgrounds. If you have a respiratory syncytial virus (RSV) journey to share, reach out here to learn more about how your voice can help spread awareness and inspire individuals from all walks of life.
We have finally reached autumn—and with the change in seasons comes a variety of common viral infections that typically emerge during this time. While many illnesses are attributed to the cold or flu—or, over the past few years, the coronavirus pandemic—there is another common virus that people need to be aware of: respiratory syncytial virus (RSV).
Historically, RSV has been considered a “childhood illness,” reports HealthPartners, because a majority of children contract the virus before their second birthday. In some individuals, RSV may be misdiagnosed as the common cold. While doctors can, and may, run tests to confirm RSV, this is often not done unless the infection is severe. Learn more about the differences in symptoms between RSV, the flu, and the common cold.
However, a number of health disparities prevent people from receiving adequate care and better outcomes. For example, conversations around RSV often fail to consider the significant impact of this illness on:
- Individuals ages 60+
- People from diverse ethnic and racial backgrounds
Failing to examine these disparities more deeply and identify potential solutions means that people face increased hospitalizations, complications, and death. In other words, this is a common condition that is underreported in certain demographics, can have severe health effects and also occupies a cultural blind spot in the general mindset of “cold and flu season.” Because of this, it is more important than ever to raise awareness about RSV and make strides to reduce the risk of serious illness.
About RSV
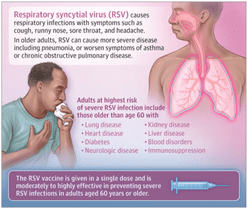
The National Foundation for Infectious Diseases explains that RSV is a common respiratory virus that infects the nose, lungs, throat, and breathing passages. You can reduce the spread of RSV by avoiding close contact with sick individuals, cleaning and sanitizing frequently used surfaces, and frequent hand-washing with soap and water. People with the highest risk of contracting severe RSV include:
- Premature infants
- Infants ages 6 months or younger
- Immunocompromised individuals
- Older individuals
Symptoms often appear within 2-8 days following infection and can include a runny nose, coughing, wheezing, sneezing, appetite loss, and a high fever. Severe RSV can lead to pneumonia or bronchiolitis (respiratory tract inflammation) in both older adults and children. If someone begins experiencing the following symptoms, please seek medical attention as soon as possible:
- High fever
- Dehydration
- Worsening cough
- Difficult, shallow, and rapid breathing
- Loud wheezing
- Bluish skin, mouth, lips, and fingernails
- Nasal flaring (in infants)
Considerations for RSV in Older Adults
If they are aware of RSV, many people still view it as a viral infection that solely or predominantly affects infants. Changing this narrative is crucial to ensuring that those affected, particularly with severe disease, receive the help that they need.
So, here’s what you should know about RSV in adults ages 60 and older:
- For most healthy adults, RSV infection clears up in about 1-2 weeks. However, in those who are older and/or immunocompromised, infection can last for up to 4 weeks.
- RSV can lead to severe complications such as pneumonia, bronchiolitis, congestive heart failure, and worsening asthma or chronic obstructive pulmonary disease (COPD).
- Each year, an estimated 60,000 – 160,000 hospitalizations in older adults are attributed to RSV across the United States. However, some people believe that this disease burden can be higher if we consider that RSV is most likely underreported.
- In November 2022, the rate of RSV-related hospitalizations in older adults was 10x higher than normal for that point in the year, reports Fortune Well.
- An article from Amy Dusto of Johns Hopkins shared that severe RSV infections also increased the risk of secondary bacterial infections.
- Up to 33% of older adults with RSV may require hospitalization.
- An estimated 6,000 – 14,000 older adults in the United States die each year due to RSV.
The CDC recommends that everyone aged 60 and older should receive a vaccination against RSV. If you are interested in getting vaccinated about RSV, please speak with your healthcare provider to determine if that is the best line of protection for you. Learn more about the RSV vaccination here.
(photo source: https://jamanetwork.com/journals/jama/fullarticle/2809541)
Ethnic Disparities in RSV—Why We Need to Talk About It
While it is important to expand the narrative around RSV to include older adults more definitively, it is also necessary to combat the racial and ethnic health disparities associated with RSV.
This disparity is clear in children. Each year, an estimated 58,000-80,000 children younger than age 5 are hospitalized due to RSV, leading to 100-300 deaths. Studies from the American Journal of Epidemiology and the Journal of Infectious Diseases, as well as a peer-reviewed consensus paper from the National Medical Association and the National Black Nurses Association and a non-peer-reviewed article in medRXiv found that children who contracted RSV were often black or Hispanic. In addition, mortality rates were highest in premature infants (African-American women are at a higher risk of giving birth prematurely) and American Indian or Alaskan Native infants, and that these children often came from families that faced insurance struggles.
However, these narratives still fail to consider the impact of RSV on adults within historically excluded and marginalized groups. Few studies have set out to explore how RSV infection, hospitalizations, and demographics are stratified based on demographics; many studies, instead, focus solely on younger, white individuals.
But the studies that have been performed discovered some sobering findings:
- In PLOS ONE, Prasad et. al explored the health and economic burden of RSV-associated hospitalizations of adults in Australia. The study found that being of Māori or Pacific Islander ethnicity, or living in a low socioeconomic status neighborhood, both correlated with increased RSV hospitalization rates.
- In the United States, Moran et. al found that hospitalization rates were higher in black children than white children. In adults, disparities also existed in relation to maternal unemployment, younger maternal age, high population density, household crowding, and socioeconomic status—all which are risk factors for RSV hospital admission.
Addressing the racial and ethnic disparities in RSV requires a multi-pronged approach. First, there needs to be more awareness raised about RSV and its ability to affect adults, making it so that people across the age spectrum understand their risks. Next, providers who work with diverse communities and historically marginalized individuals should offer more information about preventative care and vaccinations. Finally, we should seek to advocate for a more equitable health system to address these needs.
Editor’s Note: Chronic conditions and rare diseases don’t discriminate. Patient Worthy and its partners are interested in amplifying the voices of those from all identities and backgrounds. If you have a respiratory syncytial virus (RSV) journey to share, reach out here to learn more about how your voice can help spread awareness and inspire individuals from all walks of life.






