In Prohealth, Marlane Quade Cook draws on her own experience with Ehlers-Danlos syndrome to question whether the medical community has enough information and education to properly diagnose all 13 subtypes of the condition. If not, then are patients with Ehlers-Danlos syndrome not being given their proper diagnosis or treatments? Marlane shares her story of why doctors need to be better educated on EDS and offers tips to improve patients’ quality of life.
Ehlers-Danlos Syndrome
Ehlers-Danlos syndrome (EDS) is a group of inherited disorders that affect connective tissue. People with EDS have defects in collagen and other protein that normally support tissue structure and function. Symptoms differ based on the subset of EDS. However, they can include:
- Soft, velvet-like, fragile, and elastic skin that tears and bruises easily. Poor healing on scars and bruises.
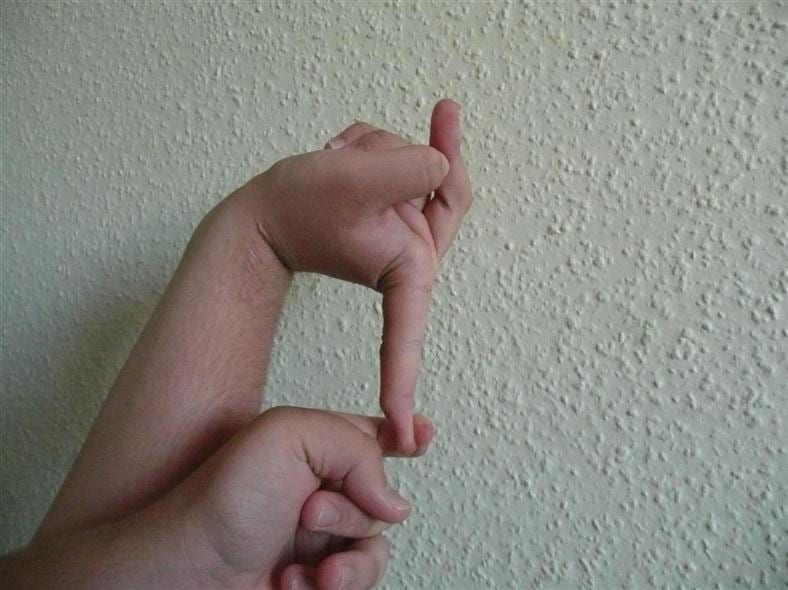
- Loose, flexible, and hyper-mobile joints that easily sprain or dislocate. Torn muscles and tendons. Deformed fingers, neck, and spine.
- Complications with and during pregnancy.
- Varicose veins.
- Abnormal heartbeats. Heart valve disease.
- Organ prolapse.
- Widespread and chronic pain.
- Internal bleeding, blood vessel rupture, and stroke.
Ehlers-Danlos syndrome can sometimes be asymptomatic until later in life. It also tends to affect people with ovaries more than those without. Some hypothesize that this is based on muscle mass. Triggers that may spur EDS symptoms also include trauma or injury, severe illness, or hormonal shifts. Symptoms may come in attacks or flares, but patients may also experience periods of “remission.”
Currently, there is no cure for EDS, but symptoms can be managed with physical therapy, braces, medications, surgery, and cardiovascular monitoring. Learn more about Ehlers-Danlos syndrome.
Marlane’s Story
Marlane was diagnosed with Hypermobile Ehlers-Danlos Syndrome (hEDS) in 2015. The Ehlers-Danlos Society notes that no single genetic mutation is currently identified as the cause of hEDS. However, if one parent has a genetic mutation for hEDS, each of their children has a 50% chance of also having the condition. In Marlane’s case, her two children and her sister have hEDS. Though they have not been tested, her mother and two other siblings also show symptoms.
Unlike Vascular EDS (vEDS) and Classic EDS (cEDS), which can cause severe or even fatal issues, Marlane notes that many doctors are not terribly concerned about hEDS. But this can be isolating. Because patients with EDS can experience anywhere from mild symptoms to extreme pain, more concern must be taken on addressing other patients. Additionally, patients with hEDS may experience comorbidities like:
- Depression
- Cancer
- Neurological issues
- POTS (postural orthostatic tachycardia syndrome)
- Autoimmune disorders
- Chronic fatigue syndrome
- Fibromyalgia
- Lyme disease
As such, Marlane advocates for patients with Ehlers-Danlos syndrome to pursue therapy, support groups, or mental health counseling if needed.
Harmful Assumptions about Ehlers-Danlos Syndrome
Although doctors do learn about EDS in medical school, Marlane notes that many solely focus on vEDS or cEDS. To better prepare the medical field to assist patients, it is crucial for doctors to be educated on the various subtypes, symptoms, and presentations of patients with EDS.
The disorder is vastly under-diagnosed and underreported. Currently, an estimated 1 in 2,500 to 1 in 5,000 people have EDS. However, a 2019 British Journal of Medicine study found that the condition may actually affect 1 in 500 people.
But the condition is also not understood outside of the medical realm. This contributes to a feeling of isolation for patients, who may hear that the condition is made up, or listen to people purposefully joke or make fun of the name of the condition. Beyond that, Marlane notes that certain medical professionals may also perpetuate myths about EDS, or minimize the impact on a patient’s quality of life.
She has heard statements such as, “You’re just flexible. That’s a good thing!” Some doctors noted, “You look fine to me,” or “So, the other day you couldn’t get out of bed, but today you can do it?”
As many patients in the rare disease community know, it can be frustrating and hurtful to search for answers only to have your experience minimized by someone who doesn’t understand. Moving forward, it is imperative to ensure that there is more patient advocacy for this community.
Tips for EDS Management
First, talk to your doctor and medical team to determine a care plan. You may want to talk to a neurologist and cardiologist to track your heart and brain function. A neurologist is especially important for patients with Ehlers-Danlos syndrome who are experiencing migraines or seizures.
Beyond that, an anti-inflammatory diet or a physical therapist could help mitigate physical symptoms. If you do look for a physical therapist, consider one who is either willing to learn about EDS and adjust their approach, or who has prior experience in this realm.