Researchers recently linked Cushing syndrome remission to the development of de novo (first occurrence) diseases, including autoimmune diseases, in various patients. But how did they reach this point?
The first step in the process, reports Dr. Patricia Inacio in Cushing’s Disease News, involved a man who was referred to an endocrinologist following one year’s worth of sleep difficulties and associated weight gain. After identifying additional symptoms—abdominal stretch marks, a buildup of fat on the neck and shoulders, undetectable ACTH levels, and elevated cortisol levels—doctors diagnosed the man with ACTH-independent Cushing syndrome. The man later had surgery to remove his left adrenal gland, where a mass had developed.
Despite treatment, the man later developed joint and muscle pain and stiffness, a tingling or “pins and needles” sensation in his extremities, muscle weakness, fatigue, headaches, and general malaise. Blood work showed that the man had swollen lymph nodes and low cortisol levels. After performing additional tests, the man was given a new diagnosis: pulmonary sarcoidosis. Doctors treated him with 20 mg hydrocortisone and glucocorticoid replacement therapy, which he was able to stop two years later.
De Novo Conditions: What Happened?
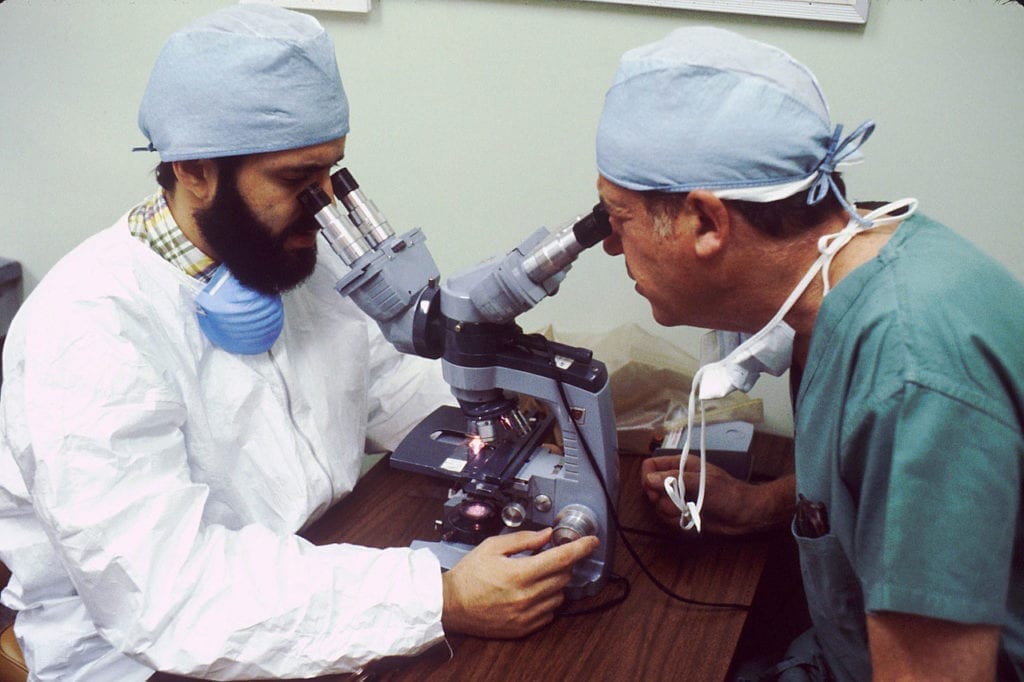
Fascinated by this case, researchers from the University of Calgary wanted to understand the prevalence of de novo conditions following Cushing remission. The research team performed a systematic literature review, the results of which were published in Endocrinology, Diabetes & Metabolism. After reviewing 43 studies, the researchers found 84 cases of de novo conditions that manifested within one year of remission. Findings show that:
- 85% of the cases identified in the literature occurred in females.
- De novo conditions include thyroid disorders (48.8%) and rheumatologic disorders (26.2%). Sarcoidosis was identified in 15.5% of patients.
- Most individuals who developed de novo conditions were taking corticosteroids.
- These conditions appeared in a median time of 4.1 months following Cushing syndrome remission.
This data suggests that physicians should be aware of new-onset symptoms in patients. Further, physicians should recognize the potential for new conditions to develop, so patients who are in remission from Cushing syndrome should have more oversight.
What to Know: Cushing Syndrome
Also known as: hypercortisolism
Cushing syndrome is a condition that occurs when your body produces too much of a hormone called cortisol. Cortisol is sometimes called the “stress hormone.” It plays an essential role in blood pressure maintenance, blood sugar regulation, inflammation, memory formation, respiration, and balancing salt in the body. Cushing syndrome is usually the result of a tumor or mass on the pituitary or adrenal glands. It is most common in people between ages 25-50 and occurs more often in women than men. Signs and symptoms include:
- A fatty lump on the back of the neck and shoulders
- Weight gain
- Red/purple stretch marks
- Fatigue
- Erectile dysfunction
- Muscle weakness
- Glucose intolerance
- Bone loss
- High blood pressure
- Rounded, moon-shaped face
- Thin, easily bruised skin
- Acne
- Extra facial/body hair in people assigned female at birth
- Absent or irregular menstruation
There are subtypes of Cushing syndrome such as Cushing disease.