Recently, researchers from European Molecular Biology Laboratory (EMBL) looked to understand the cause of pulmonary arterial hypertension (PAH). They collaborated with Stanford University through the Life Sciences Alliance. Because most (though not all) PAH cases are not caused by known gene mutations, researchers pursued potential epigenetic causes. Check out their full findings in Nature Communications.
Pulmonary Arterial Hypertension (PAH)
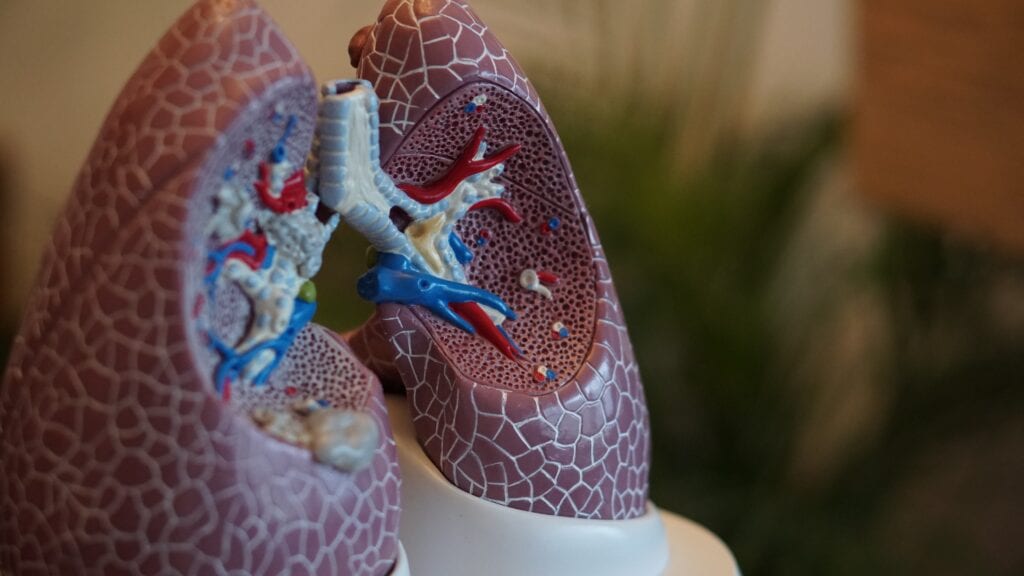
Pulmonary arterial hypertension (PAH) is a chronic and progressively worsening type of high blood pressure in the lungs. Blood pressure measures how your body is circulating and moving oxygenated and deoxygenated blood. Any pressure about 25 mm Hg (millimeters of mercury) at rest receives a diagnosis of pulmonary hypertension.
PAH causes pulmonary arteries to thicken or harden, causing issues with circulation, oxygen, and organ function. The heart needs to work harder to force blood through, and receive oxygen from, narrow arteries. In addition to weakening and damaging the heart muscle, the body also doesn’t receive enough oxygenated blood. PAH is 2x more common in women, and usually occurs between ages 30 and 60.
In some cases, a mutated BMPR2 gene causes PAH. However, it can also result from liver or lung diseases, sickle cell disease, HIV, congenital heart disease, or autoimmune diseases. Symptoms of PAH include chest pain, fatigue, swelling in the lower extremities, dizziness, and shortness of breath.
Learn more about PAH here.
Epigenetics
A Brief Overview
Researchers hypothesized that epigenetic changes could cause PAH. The NIH describes epigenetics as:
DNA modifications that do not change the DNA sequence [but] can affect gene activity. Epigenetic changes [determine] whether genes are turned on or off and can influence the production of proteins in certain cells.
In more basic terms, epigenetic changes can alter the way a gene is expressed or the way a gene acts. This can cause genetic disorders when:
errors in the epigenetic process, such as modifying the wrong gene or failing to add a compound to a gene, [lead] to abnormal gene activity or inactivity.
Exploring Epigenetic Causes of PAH
To begin, researchers compared lung cells of healthy individuals with lung cells of those with PAH. They found large-scale epigenetic changes which altered transcription factors and enhancers. Basically, these epigenetic alterations changed the entire genetic regulatory network.
One type of epigenetic change is chromatin modifications. Chromatin plays a key role in gene expression. Researchers explored pulmonary blood vessels cells and found epigenetic discontinuity.
Next, researchers created a tool to understand how these epigenetic changes shaped the development of PAH. Through this tool, they reconstructed a gene regulatory network. They then used their data to track the changes. When the gene regulatory network is reworked, endothelial cells change into smooth muscle cells. This changes the structure of pulmonary arteries, increasing weakening and narrowing.
Unfortunately, the researchers found no data that would help scientists create a more targeted gene therapy. However, it did present a next research step: understanding what causes the genetic rewiring, and what prompts the complete cellular switch.