“Looking back to the years before being diagnosed, I remember that therapy helped a lot. But I sometimes wonder if I would have had those issues anyway or if it was all caused by Lyme. We will never know.”
What if your personality suddenly started to change, and you had no control over it? William and Mary (W&M) student and 22-year-old Alexis Plofchan explains a very similar sensation she experienced when she was a freshman in high school—a time where she just didn’t feel quite like herself. The reason why? Not what you might expect.
“I was very calm and level-headed, very happy. The reason we noticed something was wrong was because of the way my personality changed. I was in 9th grade when we started noticing it. My parents thought ‘she’s 14, she’s going to a new school, it’s just hormones, and she’s a teenager.’”
“I went from being really calm to angry and upset all the time.”
“I remember driving back home from school with my dad one day and I just burst into tears because I was so confused at why I was so angry and not in control of how I was feeling emotionally, when I had never felt that way before. I think that was when we first acknowledged that something had been going on.
“For the first year, I just saw a therapist and I was diagnosed with depression and anxiety. We thought that was just the end-game because up to a certain point, therapy was able to help a lot.”
Devastatingly, Alexis’ diagnosis was more complex than anything her and her family imagined. For the next two-and-a-half-years, they continued hunting for an answer.
“In my first visit, my PCP tested for Lyme and everything under the sun- but everything came back negative and normal. Between mid-freshman and mid-senior year I started getting really tired on top of the depression and anxiety.
I remember sleeping for 18 hours once and waking still being exhausted.
I was tested for mono something like 10 different times. My mom got the call that I didn’t have mono for the 10th time when I was home sick one day and I burst out crying because I just wanted to know what was wrong with me. After a certain number of visits and tests with my PCP, he finally suggested to my mom that we might want to consider having me see a physiatrist because he didn’t see anything physically wrong.”
“We probably saw about six other doctors between my sophomore year and junior year. However, I don’t remember the process all that much because now, looking back, I was in a fight or flight mode.
I felt like I was not really present in my life.
I remember one doctor’s appointment I had my head in my mom’s lap the whole time because of how exhausted I was. It’s obviously a terrifying thing to say, but I don’t remember much of my sophomore year. It is almost like months of it are blacked out and I have to have someone remind me just what happened.”
Eventually, Alexis and her family found the reason behind the insidious creep of symptoms she had been experiencing.
“Almost three years from when I started not feeling well, we saw a functional medicine doctor who didn’t necessarily follow CDC guidelines with regards to the diagnosis of Lyme and other illnesses. We did all this bloodwork and cortisol testing in preparation for the three-hour doctor’s appointment where she went over all the results. She pulled up test after test that was essentially validating everything I had been feeling and telling doctors for the past three years. She would say ‘These three things would tell me xyz is happening’. For example, in the mornings, my cortisol levels would be far below the normal range but around 8pm, when normally they should level out, my cortisol levels would spike. This was the test that resonated with me the most because it explained my fatigue and inability to fall asleep- which at this time was the most present of my symptoms. I remember feeling really happy and positive throughout most of that appointment- like I had figured it out and it would be all uphill from there on out.
Then, in the last ten minutes, she said ‘Oh and then Lyme disease would cause this,’ and we were like ‘What?!’ And she said ‘Oh yeah, did I not say that? You have Lyme disease.’”
After Alexis’ diagnosis, she and her doctor attacked the problem the only way they knew how: long-term antibiotics.
“My doctor was doing an apprenticeship/partnership with a Lyme doctor that was in our area, who I never met in person, but who was helping my doctor with her Lyme patients. So we stuck with this functional medicine doctor, whose approach to treating Lyme was antibiotics. I took antibiotics for 18 months straight, without many breaks. Looking back and knowing what I know now about antibiotics, that probably wasn’t the best idea for my body. It would have been much better to do what I do now which is pulsing (pulsing is when you take antibiotics a few days a week with a few weeks off). But for 18 months, I was doing Doxycycline on top of Flagyl, consistently 7 days per week, all of the time.”
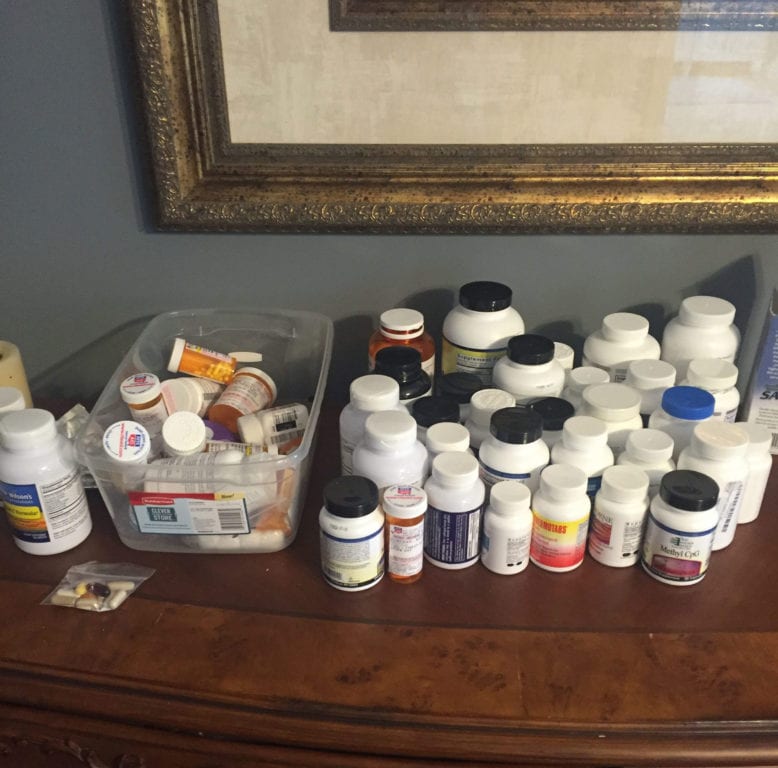
“I was also on a lot of supplements and to this day still take about 54 supplemental pills each day. A lot of the testing that my doctor had me do showed that I needed a lot of neurotransmitter help- so the supplements she gave me were aimed to help balance those out as well as my adrenals and thyroid. I also changed my diet as another part of my treatment. I came off gluten—I say that lightly– I didn’t actually get off gluten until I was a sophomore in college, but I tried to take it out of my diet as much as I could. But that was really what we did.”
It was at this point that Alexis started to see changes in how Lyme affected her.
“I can kind of look at Lyme diseases in a few different stages: Until I went to college I had depression, anxiety, exhaustion and focus issues– the last of which took a few years for me to realize the magnitude of the issues. Looking back I had other symptoms like joint pain, stiffness, etc. but I didn’t notice them as much because they weren’t the most prevalent and I was not as in tune with my body and symptoms. But then, when I went to college, my symptoms turned much more physical. I had a lot of restless leg, I couldn’t fall asleep, I had horrible headaches, and I was super stiff most of the day. Walking wasn’t necessarily hard once I got going but it was an exhausting task to think about. I lived in the furthest dorm from campus and I cannot count the times I would wake up and dread walking to class because it just physically was going to be too exhausting.
The thought of walking to class made me instantly tired and drained. It would take a while for me to get up out of bed.”
While Alexis was on treatment, she experienced what a lot of people suffering from Lyme do: a worsening of symptoms.
“I think it was spring of my freshman year in college when we decided to come off of all antibiotics in order to see where I leveled out. In the beginning the antibiotics helped in very noticeable ways. However, at that point in time the side effects of the antibiotics were up to par to what my symptoms of Lyme were. The antibiotics weren’t helping me progress anymore and most of the time they were making me sicker because of their side effects.”
“This is of course a learning process, but it’s insane looking back at the fact that we did no pulsing, whatsoever and I just attacked my system completely horribly, horribly, horribly for 18 months with some pretty strong and toxic antibiotics. “
“I took a break from antibiotics for a month and I remember calling my brother and being like ‘Tommy, holy crap I feel like myself for the first time in four years!’ It was a very surreal feeling of watching myself in my day to day life and seeing things that I had lost personality-wise and energy-wise come back. It was like I became myself again but in some ways, I had forgotten what it meant to feel myself.”
Unfortunately, the advantages of the hiatus from antibiotics didn’t last long. In searching for a path forward, Alexis felt that long-term antibiotics didn’t work for her and wanted to explore other routes for treatment.
“I caught a common cold that was going through my dorm around the end of my freshman year, and I never really bounced back. When I came back home for the summer, we took some time to determine what the game-plan was going to be. We almost took a completely herbal route through a doctor—the doctor who I am seeing now. I really didn’t want to go on antibiotics, my dad was really against them, and my mom wasn’t 100% for them either mostly because of how badly I had felt on them previously. But I knew going into the first appointment that this doctor usually used antibiotics.”
“The doctor laid it out for me, explaining that they pulsed antibiotics as opposed to taking them every day and had off weeks of no antibiotics in order to give the body a break. So I came back from that appointment and decided that was what I wanted to do. This was probably the first time I took a very active role in my treatment in the sense that I was making the decision and understood what it meant.”
“I started with her – I think it was early fall or winter of 2013, right around the time I transferred to W&M where I go now- and I have been with that office since then, doing many different types of treatments.”
Going through grueling antibiotic treatment and not seeing results is incredibly discouraging. But Alexis wasn’t about to give up. She bravely re-tried antibiotics, and also completed an alternative treatment in conjunction with the meds. This could possibly be the largest factor in her success with treatment today.
“I took off spring semester of what should have been my junior year. I had thought about taking a semester off every semester while at W&M. So for a year and a half, I would end each semester drained, usually having to reschedule exams because of being too sick, and would think ‘should I do something different, am I too sick?’ I am not sure what finally made me take that leap but I did and it was enormously impactful. I kind of took a breath and step back from school to focus completely on my health. All semester and for most of the summer, I saw my chiropractor twice a week, my acupuncturist once a week, my Lyme specialist ever 4 weeks, my therapist once a week and another Lyme doctor once a week. I was focusing all my energy on my health. I refocused my mindset on the whole ordeal and in doing so, refocused my approach for treatment.
“I also did Hyperberic Oxygen Treatment (HBOT) with my doctor as well during this time. I think that was one of the biggest treatments where I noticed it actually helping in real time. That really helped with my cognitive ability to focus, think and put thoughts together.”
Progress wasn’t instantaneous, however.
“Toward the end of the 20 treatments of HBOT is when I started noticing the improvements in my brain. If I remember correctly, I think I got worse in terms of exhaustion; I definitely relapsed a little bit because of it. I would nap the whole time I was in there. But after another 20 treatments, I could say without a doubt that it helped me regain some of my cognitive ability.”
With Alexis’ determination she continues to make tremendous strides in her treatment. But in an unfortunate twist, she’s not alone in her fight to get well.
“Right now my protocol is: two weeks on [antibiotics] and one week off. And my mom is the opposite of that. My mom is the opposite of that because she’s getting better even faster than I am in terms of the ability to come off antibiotics sooner.”

That’s right. Both of Alexis’ parents have Lyme and together, they have been navigating the difficulties of Lyme as a family. Stay tuned for part 2 of Alexis’ interview to hear their story on battling this disease as a unit.
Share Part 1 of Alexis’ story for Lyme Disease Awareness Month this May!


