Last night, I texted my mom to ask what blood type I was. “Type A, I think? I’ll have to check. Why?” she texted back. Well, I had just read an article explaining that people with Type A blood might be more susceptible to severe respiratory reactions if they developed COVID-19.
Recently, a group of 120 European research began genomic studies to understand how genetics contribute to certain COVID-19 reactions. For example, why do some people have no symptoms while others experience a severe immune reaction? Now, it seems as though genes – particularly those which control blood type – may actually play a big role. You can find the full study results published in medRxiv.
What Does Type A Blood Mean?
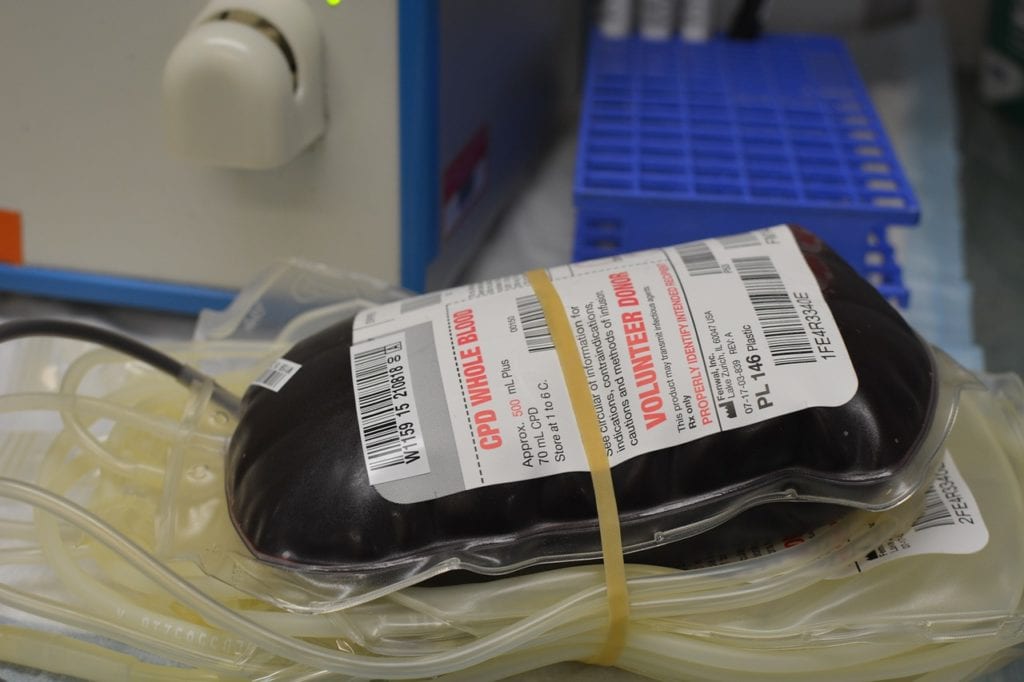
Before we start, let’s examine what blood types are and what they mean. There are four main blood types: A, AB, B, and O. These can be either positive or negative, based on whether or not you have an antigen called rH factor.
Type AB positive blood is a universal recipient, meaning people with this blood type can receive donations from any other blood type. Type O negative, on the other hand, is the universal donor, meaning it can be donated to anybody.
In the United States, 36% of people have Type A positive blood, with 6% having Type A negative blood. If you have Type A blood, you also have anti-B antibodies. Basically, you cannot receive Type B blood because the antibodies will view it as a foreign agent and attack it.
COVID-19 and the Need for Research
Towards the end of 2019, a novel coronavirus outbreak occurred in Wuhan, China. Since then, it has spread to 213 countries and territories across the globe. As of the afternoon of June 5, 2020, there are around 6.42 million positive diagnoses with 383,000 fatalities.
At first, symptoms seemed relatively straightforward: fever, body aches, a dry and painful cough, loss of smell and taste. However, as the pandemic was declared in March and more people began to come down with the illness, additional concerns appeared. Children began developing inflammatory conditions. When blood clots formed, people in their 30’s began having strokes. Most worrying, some people were having severe respiratory reactions resulting in pneumonia and a need for ventilation. Only 10% of people experienced this. Yet, a huge question loomed: why them? Why these people?
Old age, diabetes, obesity, hypertension, cardiovascular disease, and other health issues raise the risk factor. However, people still questioned whether this reaction was caused by an overactive immune system or some other unknown element.
Genomic Studies
European researchers wanted to understand whether genetics played a role in COVID-19 reactions. Initially, their study included 1,980 patients with respiratory failure caused by COVID-19. These patients were recruited from 5 hard-hit cities in Italy and Spain. However, the patient population was eventually reduced to:
- 1,610 patients
- 48% (775 patients) were from Spain. 52% (835 patients) were from Italy.
- 2,205 controls
- 43% (950 controls) were from Spain. 57% (1,255 controls) were from Italy.
Next, researchers analyzed 8,582,968 single-nucleotide polymorphisms (SNPs). According to the Genetics Home Reference, SNPs are:
the most common type of genetic variation among people, [where] each SNP represents a difference in a single DNA building block, called a nucleotide. For example, a SNP may replace the nucleotide cytosine (C) with the nucleotide thymine (T).
Additionally, the Genetics Home Reference continues that SNPs commonly occur maybe once in every 1,000 nucleotides. But while:
most SNPs have no effect on health or development, [some] of these genetic differences have proven to be very important in the study of human health. Researchers have found SNPs that may predict an individual’s response to certain drugs, susceptibility to environmental factors…, risk of developing particular diseases, [and] the inheritance of disease genes within families.
Findings: Type A Blood
First, the researchers noticed a cross-replicating association between the SNPs from chromosome 3 and 9. Further examination showed something unique about chromosome 3p21: a collection of genes that might play a role in COVID-19 infection.
The SLC6A20 gene is responsible for a transporter protein. Ultimately, this protein plays a role in angiotensin-converting enzyme 2 (ACE2). So why is this important? COVID-19 uses ACE2 to enter and infect the body. In the lungs, the protein is called Sodium/Imino-acid Transporter 1 (SIT1) is expressed in pneumocytes, the surface cells of alveoli. For future research, scientists may want to look at how SIT1 plays a role in pulmonary infection.
Additionally, researchers found a SNP on chromosome 9 that rested at the position where blood type is determined. When tested, they discovered a distinct difference between 2 blood types:
- Type O blood: People with Type O blood are 35% less likely to develop respiratory failure.
- Type A blood: People with Type A blood are 45% more likely to develop respiratory failure.
As a result, people with Type A blood are more likely to have negative effects from COVID-19. Additionally, similar findings on Type A blood were found in the 2002-2003 SARS epidemic.