According to an NBC AP news item, early results show that CRISPR, a “tool” that alters DNA permanently in blood cells, has the potential to not only stop the progression of sickle cell disease and beta thalassemia, but possibly provide a cure for both diseases.
A Look at the Initial Results
Initial results were presented this week at the 2020 ASH conference, while other results of the trial were published in the NEJM. Doctors presented the patient profiles of ten people who were administered the experimental drug called CTXOO1.
All patients who were treated with CTXOO1 were blood-transfusion independent and free from the constant bouts of pain they had experienced for so many years.
Victoria Gray of Forest, Mississippi, was the first patient who enrolled in the sickle cell trial. Victoria, age 35, described her multiple forms of pain as a plague that followed her all her life. Victoria said that the pain was so severe it often required a hospital stay.
But since her treatment with CTXOO1 a year ago, Victoria has been able to taper off her pain medication. This, she said, is what she has prayed for all her life. Victoria added that she also prays for other sickle cell patients to have the same results.
About Beta Thalassemia and Sickle Cell
While millions of people are affected by sickle cell, beta thalassemia affects one person in 100,000. Currently, the only cure is via bone marrow transplant, preferably from a sibling. The donor must be a close match and free of the disease.
The other similarity is that the mutations occur in red blood cells, the cells that transport oxygen to all parts of the body.
Presenting the Differences
The defects in hemoglobin cause deformed blood cells in SCD that do not transport oxygen properly. This results in clogged vessels, strokes, and organ damage.
In beta thalassemia there is a lack of hemoglobin. As a result, patients experience shortness of breath, anemia, and fatigue. A patient with severe symptoms will require frequent transfusions.
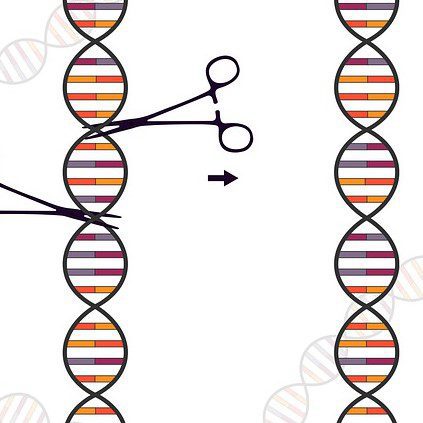
About CRISPR Editing
The CRISPR study focuses on the defects in adult hemoglobin. A specific form of hemoglobin is made in the womb. When a baby begins to breathe on its own, a gene gives instructions to cells to make an adult type of hemoglobin (the switching gene). The adult hemoglobin becomes defective in either of the aforementioned diseases. CRISPR editing is designed to cut out this switching gene.
Haydar Frangoul M.D., one of the study leaders, explains that by turning that “switch” off the cells are, in effect, back in utero. This causes them to again create fetal hemoglobin.
Dr. Frangoul commented that to date, the CRISPR technique appears to be working as they had planned. There were no unintended adverse reactions. He said that early results were very encouraging.
About the Treatment
The first step in CRISPR therapy is to remove stem cells from a patient’s blood. The CRISPR technique is then used in-vitro (in the lab) and the switching gene is eliminated.
In addition, doctors use a potent drug to kill the patient’s other defective cells that are responsible for the production of blood.
The patients are then infused with their own cells that had been re-engineered in the lab.
The First Study Participants
The recent results involved seven patients (including one seven-year-old) who were diagnosed with beta thalassemia, as well as three sickle cell patients.
The participants received CRISPR therapy. As discussed, the treatment involved the removal and re-engineering of stem cells in order to turn off the switching gene.
None of the patients reported pain after the treatment. Transfusions were no longer necessary for five of the six patients. Hemoglobin levels in these patients returned to near normal.
The trial sponsors and developers, CRISPR Therapeutics of Switzerland and Vertex Pharmaceuticals based in Massachusetts, plan to expand their current studies in the U.S. and Europe with forty-five participants in each location. Currently, the trials for each disease are being run separately.
About the Competition
Bluebird Bio’s Beti-cel is a strong competitor of the Vertex and CRISPR therapy. David Williams M.D. of the Children’s Hospital in Boston, Massachusetts announced partial results of their study after testing its unique form of gene therapy.
The study, designed to establish safety, is funded through government grants. Its goal is to restore the production of fetal hemoglobin for people with sickle cell. Bluebird has provided the study’s therapy. The team will enroll a total of ten people. A study to test its efficacy will take place at a later date.
Dr. Williams agreed that Dr. Frangoul’s study confirms using the approach to attack sickle cell by way of the hemoglobin’s switching gene.