Although the medical field has made significant strides over the years, there is still a lot we don’t know about the body. For example, what can we learn about ourselves—or our diseases—from certain biomarkers? How do elevated inflammatory markers like platelet-to-hemoglobin ratio (PHR) or platelet-to-lymphocyte ratio (PLR) provide insight into what we’re feeling? In an article published in Scleroderma News, Dr. Lindsey Shapiro, PhD dives into the second question; a study published in Reumatologia Clinica found that elevated PHR and PLR were linked to greater or worsening disease activity in patients living with systemic sclerosis.
Evaluating the Research
The research team focused on PLR and PHR because of their underlying mechanisms. Inflammation, blood vessel damage, and fibrosis are all hallmarks of systemic sclerosis. Evaluating PLR and PHR provide markers of these processes within the body.
In this particular study, an Egyptian research team wanted to understand the relationship between PLR, PHR, and disease manifestation. Altogether, 60 patients enrolled. A large majority were female. The mean PHR was 32.96, with the mean PLR sitting at 245.07. Findings from the study show:
- That elevated PLR level was consistent with prior research and reporting on the relationship between PLR and inflammatory disease states.
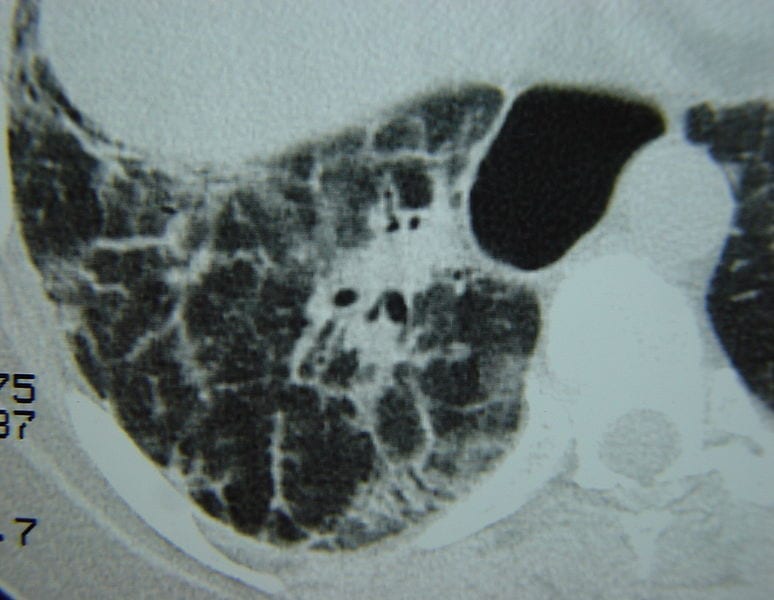
- High PLR and PHR were both associated with musculoskeletal issues, pulmonary issues, and skin ulcer formation.
- There were no differences in PLR or PHR in groups using or not using immunosuppressive therapies.
- Both PLR and PHR were positively correlated with higher disease activity and certain biomarkers associated with bodily inflammation.
Ultimately, the research team found that PLR levels over 107.8, or PHR levels over 23.5, could predict worse disease activity in patients with systemic sclerosis. However, the researchers also note that additional confirmatory testing is needed.
An Overview of Systemic Sclerosis (SSc)
Also known as systemic scleroderma, systemic sclerosis is an autoimmune disorder characterized by fibrosis (scar tissue formation) in the skin and internal organs. As a result, the skin becomes thickened. While localized sclerosis affects only certain parts of the body, systemic sclerosis may also affect internal organs. It is significantly more common in females than males.
Symptoms, which often appear in middle age, may include diarrhea; joint pain; shortness of breath; high blood pressure; difficulty swallowing; heartburn; painful calcium deposits beneath the skin; open sores on the fingers; Raynaud’s phenomenon; kidney issues; hardened or tightened skin patches; or swollen hands and fingers. If the fibrosis does affect the organs, it can also lead to impaired function or even organ failure.
Right now, no cure exists for people living with systemic scleroderma. However, there are treatment options available that can aid in symptom management. These include blood pressure or pain relief medications, physical therapy, antibiotics, or anti-fibrotics (among others).