Welcome to the Rare Classroom, a new series from Patient Worthy. Rare Classroom is designed for the curious reader who wants to get informed on some of the rarest, most mysterious diseases and conditions. There are thousands of rare diseases out there, but only a very small number of them have viable treatments and regularly make the news. This series is an opportunity to learn the basics about some of the diseases that almost no one hears much about or that we otherwise haven’t been able to report on very often.
Eyes front and ears open. Class is now in session.
The disease that we will be learning about today is:
Scleroderma
This rare disease is also known as systemic scleroderma, systemic sclerosis, or diffuse scleroderma.
What is Scleroderma?
- Scleroderma is a chronic connective tissue disease generally classified as one of the autoimmune rheumatic diseases
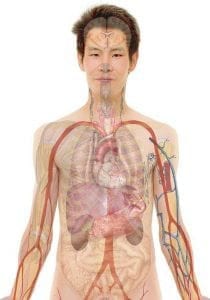
- It can involve the skin, esophagus, gastrointestinal tract, lungs, kidneys, heart and other internal organs. The connective tissues of involved organs become hard and fibrous, causing them to function less efficiently.
- It’s estimated that about 300,000 Americans have scleroderma. About one third of those people have the systemic form of scleroderma.
- Diagnosed in approximately 67 male patients and 265 female patients per 100,000 people each year
- Diagnosis may require consultation with rheumatologists, and/or dermatologists and require blood studies and numerous other specialized tests depending upon which organs are affected.
- Type of treatment depends on the severity of the disease and the complexity of symptoms
- Scleroderma is classified as localized or systemic; systemic sclerosis is classified as limited or diffuse
- Annual direct and indirect costs of SSc in the United States are $1.5 billion
- The high cost of SSc, despite its low prevalence, suggests that the burden of rare chronic diseases can be high.
- The high morbidity costs reflect the young age of onset of the disease as well as the need for treatments to decrease morbidity costs.
- Approximately 15 percent to 25 percent of people with features of systemic scleroderma also have signs and symptoms of another condition that affects connective tissue, such as polymyositis, dermatomyositis, rheumatoid arthritis, Sjögren syndrome, or systemic lupus erythematosus. The combination of systemic scleroderma with other connective tissue abnormalities is known as scleroderma overlap syndrome.
How Do You Get It?
- Like with many other rare diseases, the exact cause remains unknown
- Risk factors include:
- Abnormal immune or inflammatory activity
- Scleroderma is believed to be autoimmune in nature. In scleroderma, the immune system is thought to stimulate cells called fibroblasts, so they produce too much collagen. The collagen forms thick connective tissue that builds up within the skin and internal organs and can interfere with their functioning.
- Genetic makeup
- Genes seem to put certain people at risk for scleroderma and play a role in its course. The disease is not passed from parent to child like some genetic diseases.
- Environmental triggers
- Exposure to some environmental factors may trigger scleroderma-like disease (which is not actually scleroderma). No environmental agent has been shown to cause scleroderma. In the past, some people believed that silicone breast implants might have been a factor in developing connective tissue diseases such as scleroderma. But several studies have not shown evidence of a connection.
- Hormones
- Females develop scleroderma more often than males. Scientists suspect that hormonal differences between the two play a part in the disease
- Abnormal immune or inflammatory activity
What Are the Symptoms?
- Early symptoms include:
- Swelling then thickening and tightening of the skin at the ends of the fingers
- Raynaud Phenomenon
- Heartburn
- Difficulty Swallowing
- Shortness of breath
- Aches and pains in joints
- Muscle pain and weakness
- Skin:
- Hardening and tightening of patches of skin
- Skin can appear shiny because it’s so tight, and movement of the affected area may be restricted
- Joints:
- Fingers, wrists, and elbows may become stuck (forming a contracture) in flexed positions because of scarring in the skin
- Digestive system:
- Damage to the esophagus can cause swallowing difficulties and heartburn
- Abnormal cell growth in the esophagus (Barrett esophagus) occurs in about one third of people, increasing their risk of esophageal blockage due to a fibrous band or their risk of esophageal cancer
- Damage to the intestines can interfere with food absorption and cause weight loss
- Heart:
- Heart failure
- Arrhythmias
- Kidneys:
- Kidney damage
- Scleroderma renal crisis – This is the acute onset of renal failure and hypertension. Scleroderma renal crisis can be life-threatening.
- Lungs:
- Scar tissue accumulating in the lungs can cause interstitial lung disease causing shortness of breath
- Blood pressure increases due to blood vessel damage can cause pulmonary hypertension
- Several types of lung disease may develop in people with systemic scleroderma with lung involvement
- Interstitial lung disease (ILD) and pulmonary arterial hypertension (PAH) are the two most common and severe types of lung disease, and are leading causes of death in scleroderma patients
- ILD develops when too much collagen accumulates in the lungs, making them stiff
- Symptoms of ILD develop gradually, with patients commonly experiencing shortness of breath and a dry cough
- Pulmonary arterial hypertension (PAH) is a condition marked by increased resistance to blood flow in the vessels supplying blood to the lungs. It may develop in scleroderma patients as a result of inflammation damaging the lining of the pulmonary arteries, causing blood vessels to narrow increasing resistance.
- People with mild PAH may experience no symptoms, but moderate to severe disease is usually marked by persistent shortness of breath, especially when exercising. PAH places a strain on the right side of the heart, and can result in right-sided heart failure if untreated.
How Is It Treated?
- There is no cure for systemic scleroderma.
- Treatment is directed at symptoms and dysfunctional organs
- There is great variation in the treatment prescribed due to differences in disease expression
- No drug significantly influences the natural course of SSc overall, but various drugs are of value in treating specific symptoms or organ systems
- Treatment is generally overseen by rheumatologists with larger medical facilities often having a scleroderma center
- Other specialists include: dermatologists, pulmonologists, nephrologists, cardiologists and orthopedic surgeons
- Medications are generally geared to: dilate blood vessels; suppress the immune system; reduce stomach acid; prevent infections, and relieve pain
- Treatments by symptom:
- Raynaud phenomenon
- Calcium Channel Blockers
- Angiotensin II Receptor Antagonists
- ACE Inhibitors
- Joint problems
- NSAIDS
- COX-2 Inhibitors
- Low-Dose Corticosteroids
- Narcotics
- Gastrointestinal reflux
- Antacids
- H2 Blockers
- Proton Pump Inhibitors
- Intestinal dysfunction
- Prokinetic Agents
- Somatostatin Agonist
- Antibiotics
- Renal involvement/high blood pressure
- ACE Inhibitors
- Pulmonary arterial hypertension
- Prostaglandin Derivatives
- Treprostinil
- Iloprost
- Endothelin Receptor Antagonists
- IP Receptor Agonist
- PDE5 inhibitors
- Pulmonary fibrosis
- Anti-Fibrotic Agent
- Tyrosine Kinase Inhibitor
- Immunosuppressants
- Alkylating Agents
- Raynaud phenomenon
- Other options include:
- Autologous Hematopoietic Stem Cell Transplantation
- A study of people with severe scleroderma found that a new approach using stem cell transplants provides a better outcome than an immune-suppressing drug
- Surgery
- Used as a last resort
- Surgical procedures that can be used for scleroderma complications include:
- Amputation
- Lung transplant
- Physical Therapy
- Autologous Hematopoietic Stem Cell Transplantation
Where Can I Learn More???
- Learn more about this disease from the Scleroderma Foundation.
- Check out our cornerstone on this disease here.