According to a recent article in the Seattle Cancer Care Alliance, the FDA’s recent approval of Axi-cel (Yescarta) will improve the chances of survival for relapsed or refractory follicular lymphoma. Currently, the five-year survival rate for patients receiving their third form of therapy is twenty percent.
Axi-cel’s approval, announced by its developer Kite Pharma, was supported by data from the NCT03105336 phase II ZUMA-5 trial. Axi-cel (axicabtagene ciloleucel) is a chimeric antigen receptor T (CAR-T) cell immunotherapy that was initially approved in 2017 for the treatment of relapsed or refractory large B-cell lymphoma. The 2017 approval included diffuse large B cell lymphoma (DLBCL) resulting from follicular lymphoma.
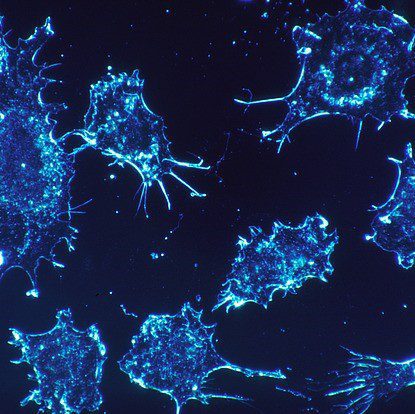
Follicular lymphoma is a cancer of the immune system and is considered a form of B-cell non-Hodgkin lymphoma. The disease is generally slow-growing (indolent). The tumor cells form in groups that turn into nodules.
The Phase II ZUMA-5 Trial
Axi-cel was evaluated in 151 slow-growing non-Hodgkin lymphoma patients who were refractory (did not respond to previous drugs) or who had relapsed after two lines of therapy. The patients had received previous diagnoses of either marginal zone lymphoma or follicular lymphoma.
Ninety-one percent of the patients who were diagnosed with relapsed or refractory follicular lymphoma (81 patients) responded to the treatment. Sixty percent of these patients achieved complete remission.
At the eighteen-month mark, 74 percent of these patients had continued remission. The median response, which is a tumor responding to treatment without progressing, was not reached.
The Safety Factor
One hundred forty-six patients were involved in the safety analysis. Eight percent of participants experienced some severe or life-threatening grade three or higher side effects, including cytokine release syndrome. Twenty-one percent of participants experienced neurological events. Yescarta prescribing information indicates warnings for these risks.
About CAR T-cell Therapy
CAR T-cell therapy is performed by extracting the cancer patient’s white blood cells and reprogramming the T cells with proteins called Chimeric Antigen Receptor (CAR). The engineered T cells are then re-infused into the patient.
The reprogrammed T cells are able to bypass the healthy cells. They bind to the diseased cells and kill them. This is the patient’s immune system fighting cancer.
A CAR T-cell Patient Defeats DLBCL
For a while, it looked like Scott Mcintyre was succumbing to DLBCL. An article by UChicago Medicine describes how he fought his way through a stem cell transplant, several different chemotherapy treatments, plus two clinical trials and targeted radiation. Remission in each case was only temporary.
Just at the point that the cancer had advanced to his lungs, his doctors suggested that he might try a new and promising immunotherapy clinical trial. The trial was conducted at UChicago.
Scott survived the procedure after having a fever for several weeks. This side effect (known as cytokine release syndrome) had been anticipated. Scott received a phone call from a UChicago Medicine oncologist a few weeks after he returned home. She gave Scott the results of the bone marrow transplant: the cancer was gone.
Christi Shaw, CEO of Kite, was quoted in a press release saying that its CAR T-cell therapy is a top priority. The company will continue to focus on patient survival and bringing hope to patients in need.