If you’re a fan of country music, you might recognize Joe Nichols’ name because of chart-busting hits like, “Gimmie That Girl,” “Sunny and 75,” and “Freaks Like Me.”
But Nichols is making a name for himself for another reason: raising awareness for idiopathic pulmonary fibrosis (IPF), the rare, incurable lung disease that claimed the life of his father.
“It started off with a very violent cough.”
Most of the tissues deep in your lungs look kind of like fine lace because the lung’s one million tiny air sacs, called “alveoli,” are thin-walled and pliant. In healthy, functioning lungs, we breathe in oxygen and then it:
- Passes through the walls of the alveoli and into nearby blood vessels
- Attaches to red blood cells that carry it to the rest of the body
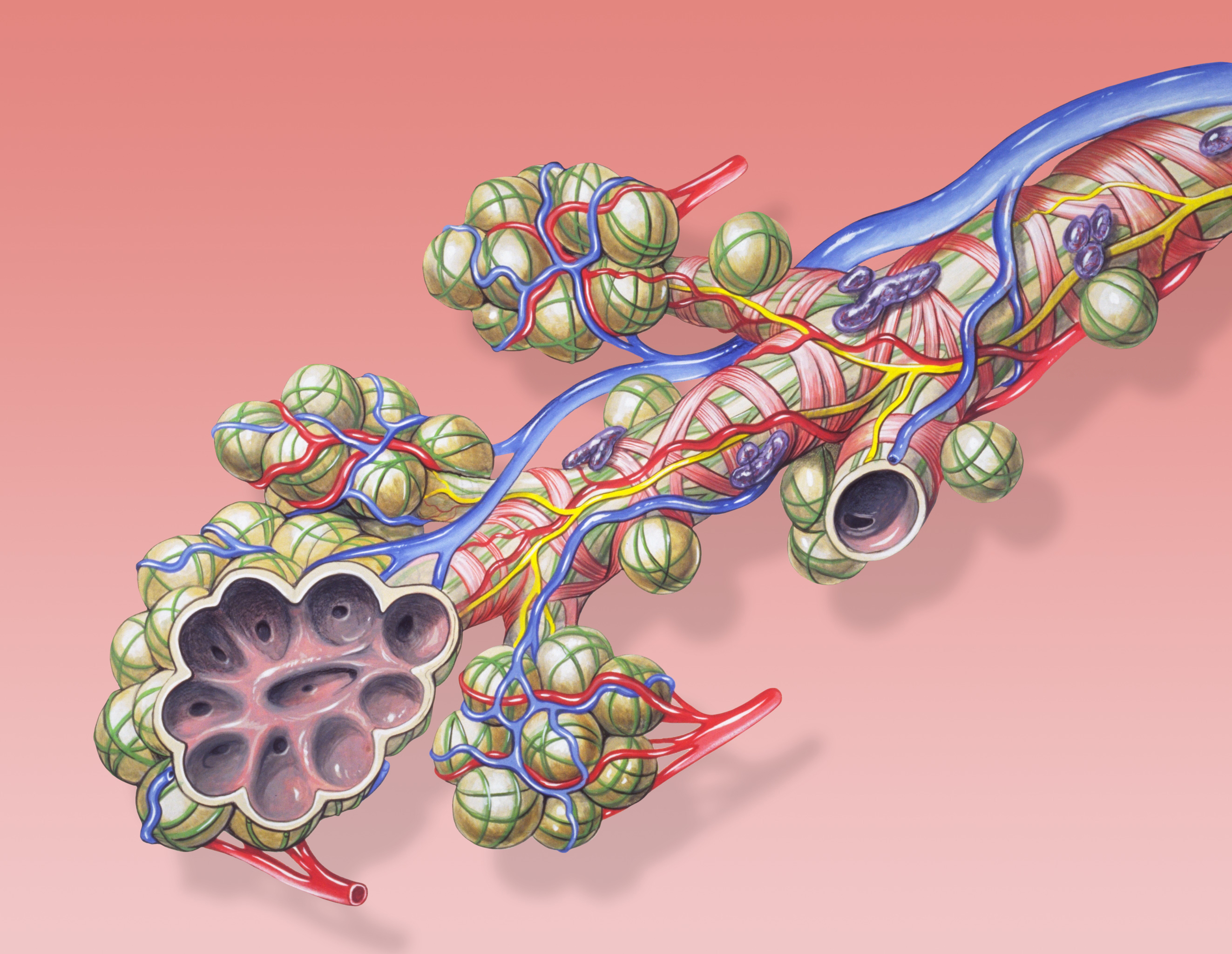
In IPF, tissues around and between (that’s what the word “interstitial” in a conversation about IPF refers to: the spaces between) the alveoli become thick and stiff with scar tissue.
“Fibrosis” is the development of fiber-like connective tissue, as in a scar. “Pulmonary” refers to the lungs. “Idiopathic” means that the cause is unknown.
Oxygen can’t easily pass through IPF-thickened tissue, decreasing the amount of oxygen getting through to vital organs, such as your heart and brain.
For years, Nichols’ father Michael, suffered from symptoms of IPF that included shortness of breath and violent coughing fits. But time after time, doctors misdiagnosed him.
IPF Misdiagnoses
After his dad’s passing, Nichols decided to honor his father’s memory by using his fame to raise awareness about IPF, a disease that carries a prognosis worse than many cancers. He has helped launch “Breathless: A Behind-the-Scenes Look at IPF,” an educational campaign that shares real people’s personal stories about the impact IPF has had on their lives.
The goal of the campaign? To teach people about IPF, increase research focusing on the disease, and empower people affected by the disease to speak up about the need for more treatments and a cure.
Nichols in particular wants to encourage others to avoid the same prolonged diagnosis experience his own father had. Diagnosing IPF is difficult—some estimates say that more than 50% of all people with IPF were initially misdiagnosed with other forms of respiratory illness.
Why? First of all, IPF is quite rare, and doctors are trained to consider common diagnoses before rare ones. There’s even medical slang for an uncommon disease: zebra, as in “When you hear hoof beats, think horse, not zebra.”

Think about it: asthma, for example, affects 20 million Americans vs. IPF’s 132,000. Some doctors may not see a single case of IPF in their entire careers.
Also, IPF shares symptoms with many other lung diseases. Early symptoms include a dry cough and getting out of breath when you exert yourself. These could also be caused by smoking habits or just plain getting older (IPF is rare before age 50), not to mention congestive heart failure or chronic obstructive pulmonary disease (COPD).
Before the FDA approval of two new treatments for IPF in 2014, lung transplantation was pretty much the only option available. None of the available treatments cure IPF, but they have been shown to slow the progression of the disease.
That’s one of the main reasons early diagnosis of IPF is so important. The earlier a person is correctly diagnosed, the earlier treatment can start to slow down it’s progression. Since the survival time for IPF is between two to five years from the time of diagnosis, it’s essential to begin curtailing disease progression ASAP.
In the BreathlessIPF campaign, Nichols discusses not only his father’s experience, but also his own quest to raise awareness about IPF. Dr. Marilyn Glassberg, a nationally-renowned University of Miami pulmonologist, joins Nichols on the video to talk about the disease from a medical perspective.
The bottom line is that the campaign wants to reach anyone who believes they, or someone they know, might have IPF and urge them to seek medical care sooner rather than later.
The campaign’s website www.BreathlessIPF.com has several resources for IPF patients and their caregivers. Nichols would love it if people who are not personally affected by the disease would still visit the website just to learn.
Breathless IPF is strongly encouraging sharing the campaign on social media because it just might reach someone in need who would not otherwise be reached, and provide them with the valuable information they need to take action or seek treatment. We encourage you to do the same. Share this post on social media and share you thoughts in the comments below!


