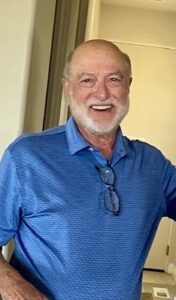
Twenty years is a long time to believe a cancer chapter has closed. For two decades after my radical prostatectomy, I lived with the quiet confidence of someone who had moved on. My PSA was undetectable for years. My doctors reassured me at every visit. I exercised daily, traveled, stayed active, and built a life that no longer included the shadow of prostate cancer. I assumed, like many men do, that the risk of recurrence faded with time.
But cancer does not always follow the timelines we imagine.
The Unexpected Return
In late 2024, more than twenty years after surgery, a small rise in PSA appeared. It was subtle but unmistakable. A PET scan revealed two pinpoint nodes along my left pelvic wall. Their size was so small that, without advanced imaging, they would have remained invisible. I underwent five sessions of highly focused radiation. Three months later, imaging confirmed that the targeted nodes had been destroyed — but two new “spots,” one near the previous site and another on the T9 transverse process, had emerged.
That was the moment I realized that prostate cancer does not operate on our psychological timelines. The disease can stay dormant for decades and then re-announce itself with surprising precision. This reality — rarely discussed with patients — is something we need to acknowledge more openly.
Starting Orgovyx: A New Chapter in Hormonal Therapy
My clinicians recommended starting relugolix (Orgovyx), an oral form of androgen deprivation therapy (ADT). I had always associated ADT with injections, long-term side effects, and profound physical changes. The idea of “medical castration,” as it is clinically defined, was emotionally jarring.
What I did not expect was the speed at which the medication worked. Within six weeks:
- My PSA dropped to undetectable.
- My testosterone fell to below zero, a result that surprised even my physicians.
These numbers brought relief. But they did not tell the whole story.
Living With ADT: What the Numbers Don’t Capture
Most clinicians know the expected side effects of ADT: hot flashes, fatigue, metabolic changes, sexual dysfunction, muscle loss, and mood fluctuations. But the lived experience is far more nuanced — and understanding it could greatly improve patient support.
- The Physiology of Sweats: A Daily Uncertainty
The first and most unpredictable symptom was sweating. It did not follow a consistent schedule. Some nights were drenched; others were peaceful. Some days were perfectly normal; others brought sudden waves of heat. Even minor triggers — a cup of salsa, a single ounce of alcohol, a different vitamin, or Tylenol taken at night — could amplify symptoms.
Patients benefit when clinicians explain that ADT destabilizes hypothalamic temperature thresholds. For me, being taught why something happens mattered more than being told that it happens.
- Maintaining Muscle Mass at 82: A Critical Success Factor
I have always been physically active. Even now, at 82, I play golf twice a week, perform structured upper- and lower-body exercises, walk daily, and monitor my performance. ADT challenges this identity. It threatens muscle integrity, energy levels, and stamina — all essential to my quality of life.
My clinicians briefly acknowledged this but did not provide specific, actionable guidance. Many older adults would benefit from structured exercise prescriptions, not merely recommendations. ADT should prompt proactive conversations about resistance training, protein intake, hydration, and recovery — the building blocks of preserving functional independence.
- Emotional and Psychological Adaptation
Something unusual happened early in my ADT course: despite being medically castrated by lab definition, I remained able to experience orgasm. This contradicted everything I had been told. Rather than dismissing it as atypical, I wish clinicians acknowledged that sexual responses vary widely, and preserving any degree of function can be emotionally stabilizing.
The psychological effects of ADT — anxiety, identity disruption, fear of progression, and the daily negotiation with one’s own body — deserve as much attention as lab values. Even a few minutes of clinician-initiated conversation can normalize a patient’s fears and reduce isolation.
Integrative Approaches: What Helped and What Needs Further Study
As someone committed to wellness, I explored several complementary approaches:
- Acupuncture: On some days it reduced sweats; on others it made me feel temporarily worse. Understanding that acupuncture may modulate autonomic balance helped me interpret these fluctuations.
- Nutrition: Daily smoothies containing soy milk, plant protein, flaxseed, aloe, and berries helped stabilize energy and bowel regularity.
- Hydration and electrolytes: Essential during high-sweat nights.
- Resistance training: The single most protective intervention for mood, metabolism, and strength.
What is missing is clinical guidance that integrates these modalities. Many ADT patients pursue them anyway; it would be beneficial for clinicians to provide structured frameworks for evaluating safety and effectiveness.
The Need for Greater Awareness: Prostate Cancer’s Silent Prevalence
One of the most surprising realizations during my journey is the disparity between awareness of prostate cancer and breast cancer. Both affect similar numbers of individuals annually, yet public messaging, funding visibility, early-detection campaigns, and survivor advocacy heavily favor breast cancer. This creates a psychological divide: women are encouraged to speak openly, while men often remain silent.
As a result, countless men are unaware of:
- Post-prostatectomy recurrence patterns
- PSA monitoring expectations
- ADT side effects
- Imaging advances
- Long-term survivorship strategies
After joining a prostate cancer support group with over 40,000 members, I was struck by how many men lack clear guidance. This is a public-health blind spot that warrants correction.
What Clinicians Can Do Differently — A Patient’s View
Based on this experience, here are five opportunities for immediate improvement in patient care:
- Normalize the possibility of very late recurrence
Not to frighten patients, but to empower them with realistic expectations.
- Provide early, structured lifestyle guidance for men starting ADT
Exercise, nutrition, and hydration programs should be standard, not optional.
- Discuss the emotional and identity-related effects openly
Men often internalize anxiety and shame; clinician-initiated dialogue matters.
- Individualize sexual-health counseling
Experiences vary more than patients are led to believe.
- Promote prostate-cancer awareness with the same energy devoted to other major cancers
Public education saves lives — and reduces the despair men feel when they believe they are alone.
Reflection: Finding Meaning in the Unexpected
I never expected to face prostate cancer again after twenty years. Yet this experience has given me a new purpose: to advocate, educate, and help others navigate a path I never imagined I would walk a second time. What I’ve learned is simple: patients don’t just need treatment — they need understanding, partnership, and a roadmap for living well through uncertainty.
If my story helps even one man prepare better, adapt faster, or feel less alone, then this recurrence may serve a greater purpose than I ever expected.
Learn more at TheProstateEducationProject.org