Unfortunately, many people with sickle cell disease are at an increased risk of experiencing central nervous system complications that can reduce quality of life. But more importantly, complications like stroke, silent cerebral infarcts (small areas of dead cerebral tissue), and cognitive decline can be extremely dangerous to your health. Recently, the American Society of Hematology (ASH) published a series of 19 recommendations on treating these complications. Check out the full set of clinical guidelines, and other recommendations, within Blood Advances.
Sickle Cell Disease
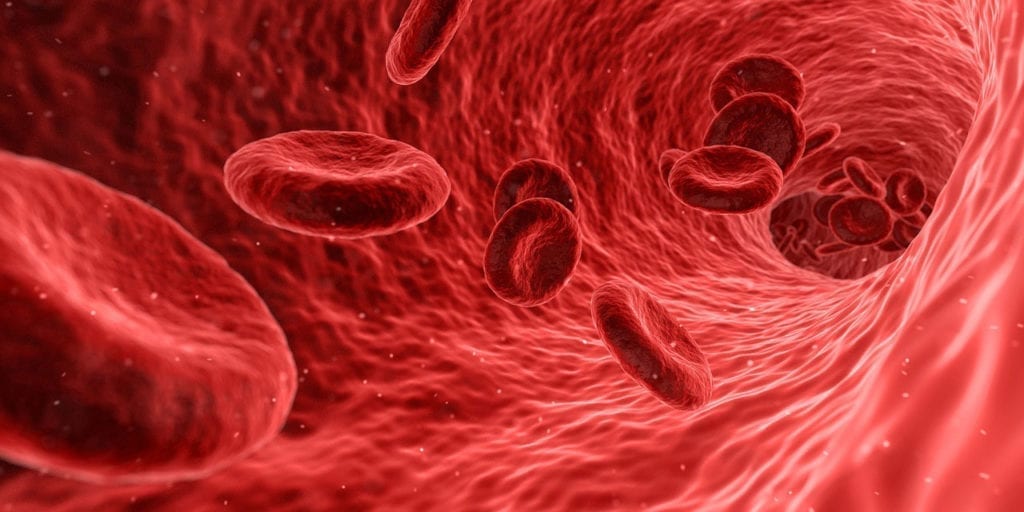
Sickle cell disease stands for a group of disorders caused by HBB gene mutations. Different mutations in the HBB gene created varied versions of beta-globin, part of the proteins that make up hemoglobin. One such mutation creates a type of beta-globing called hemoglobin S. In people with sickle cell disease, the hemoglobin S takes over one of the 4 protein subunits of hemoglobin. These abnormal hemoglobin molecules then deform red blood cells into a crescent (sickle) shape. As a result, the blood cells either die quickly or get stuck in other blood vessels.
There are many subsets of sickle cell disease, such as sickle beta-zero thalassemia and sickle cell anemia. Symptoms, and symptom onset, vary. However, they often include:
- Frequent infections
- Anemia (a low red blood cell count)
- Fatigue
- Shortness of breath
- Abnormal or delayed development
- Jaundice
- High blood pressure
- Pain
- Organ and tissue damage
- Pulmonary hypertension
Learn more about sickle cell disease.
New ASH Clinical Guidelines
To ensure that patients are receiving the highest level of care, the ASH created new clinical guidelines on preventing, diagnosing, and treating central nervous system-related complications in patients with sickle cell disease. The recommendations are also designed to create cohesive standards of care that can be implemented on a wide scale. Some of the recommendations include:
- To prevent stroke, children between the ages of 2 and 16 who have HbSS or HbSβ0 thalassemia should receive a transcranial doppler ultrasound screening (TCD screening) each year. If their blood velocity is abnormal (over 200 cm/s), then the child should receive a blood tranfusion at least once a month for a period of one year.
- However, this is dependent on whether or not the treatment is accessible in a low-middle or high-income area.
- Adults and children with sickle cell disease should receive blood transfusions within 2 hours of experiencing any neurological problems.
- Children with HbSS or HbSβ0 thalassemia should receive at least 1 MRI to check for the presence of silent cerebral infarcts.
- Parents, and clinicians, should carefully observe children to detect any early signs of developmental or cognitive delays. If any concerns arise, such as behavioral problems, issues in school, or hyperactivity, the children (and families) should be referred to a psychologist or PCP.
To read the full list of recommendations, head to Blood Advances.
The Limitations of Sickle Cell Disease Treatment Guidelines
Ultimately, the ASH’s guidelines will assist clinicians with early detection, diagnosis, and treatment of potential complications resulting from sickle cell disease. However, these guidelines do have some limitations.
First, lower or middle-income areas may not have doctors with a high level of expertise. For example, Dr. DeBraun spoke about how treating children is difficult in areas like West Africa where doctors may not have the available resources or training.
Next, cost is a factor in sickle cell disease diagnosis and treatment. These guidelines could potentially be implemented on a wider scale, creating a more cohesive standard of care. However, if patients and their families cannot afford healthcare, much less screening or therapeutic options, there is a huge barrier to overcome.
Finally, these guidelines will be most effective if clinicians implement them, but also if patients understand them. The ASH recommends that informative materials and other resources are provided to educate patients on their condition, treatments, and potential complications.
Read the original article here.